A revolutionary new wave of artificial intelligence is reshaping oncology. Recent clinical trials show that AI in cancer diagnosis is now able to detect early-stage tumors with accuracy that matches—or even exceeds—experienced radiologists.
How the AI Works
The system uses a deep convolutional neural network trained on over 1 million anonymized imaging datasets, including X-rays, MRIs, and PET scans from patients across 18 countries. This model continuously learns to identify patterns associated with various cancers—including lung, breast, and pancreatic—long before they become visible to the human eye.
It incorporates multi-modal data, combining scan results with patient history, genetic markers, and lab values to increase diagnostic accuracy.
“We’re not replacing doctors,” said Dr. Hannah Liu, lead researcher at the NCI. “We’re giving them superpowers.”
Clinical Trial Highlights
In a peer-reviewed study published in The Lancet Oncology, the AI system was tested on 10,000 high-risk patients. Here’s how it performed:
- Lung cancer: 96% detection rate (vs. 88% by radiologists)
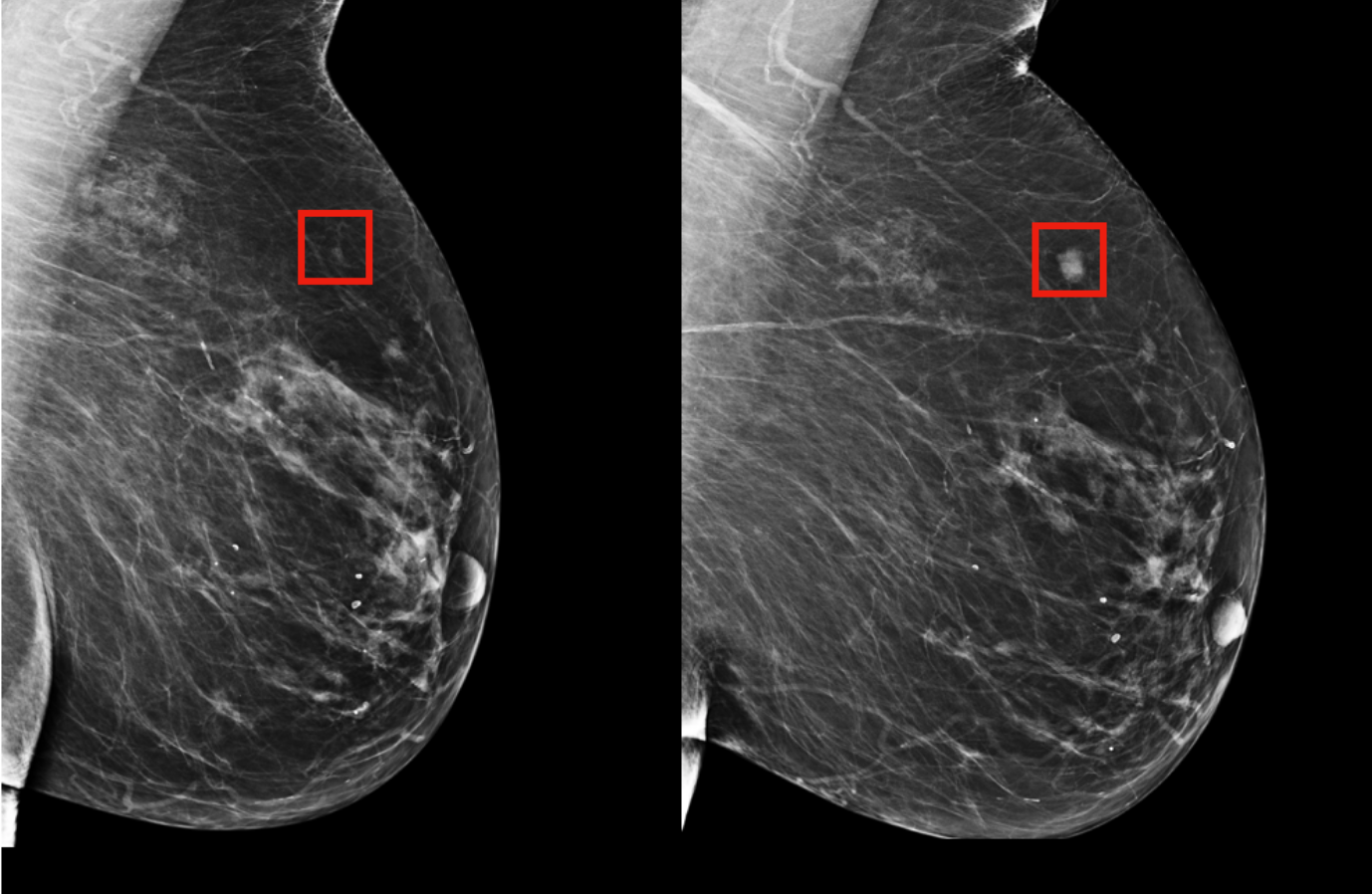
- Breast cancer: 94% detection in dense tissue scans (vs. 79% human)
- Pancreatic tumors: Detected 3–6 months earlier than traditional screening
In 7% of cases, the AI flagged anomalies that were later confirmed to be early malignancies—even when initial radiology reports showed no concerns.
Real Patient Case: Early Detection Saves a Life
In Boston, 47-year-old patient Sarah Thompson was part of an early trial. Her routine lung scan appeared normal, but the AI model flagged a minor shading discrepancy. A follow-up biopsy revealed Stage 1 lung cancer—caught months earlier than it would have been through conventional screening.
“I didn’t feel sick, and my doctors said everything looked fine,” she said. “That AI system may have saved my life.”
Benefits for Overloaded Healthcare Systems
With radiology departments under increasing pressure, AI tools offer a solution that boosts efficiency and accuracy. Benefits include:
- Faster results: AI analyzes imaging in seconds, accelerating diagnosis
- Fewer errors: Reduces missed diagnoses and false negatives
- Triage assistance: Prioritizes critical cases for immediate attention
- Scalability: Can be deployed remotely in underserved regions
Hospitals in India and Sub-Saharan Africa are already piloting the system to assist overburdened doctors in high-volume clinics.
Limitations and Ethical Concerns
Despite its promise, AI in cancer diagnosis must overcome critical hurdles:
- Bias: Models trained on non-diverse data may perform poorly across ethnicities
- Transparency: Deep learning models often operate as black boxes
- Regulation: Global healthcare agencies are still drafting AI oversight policies
- Trust: Some doctors are hesitant to rely on machines for life-altering decisions
To address this, the NCI system includes explainable AI (XAI) features that highlight exactly why a scan was flagged—adding clarity and accountability to the diagnostic process.
Integration with Hospital Systems
The AI model is currently being integrated with Electronic Health Record (EHR) systems like Epic and Cerner. This allows automated syncing of scan results, flagged anomalies, and recommended next steps directly into the physician’s workflow.
With proper permissions, these insights can also be shared securely with patients, allowing them to understand their health status and options faster than ever before.
Global Adoption on the Horizon
Countries including the UK, South Korea, and Canada are expected to approve clinical deployment of the system by 2026. In the U.S., the FDA has granted it Breakthrough Device designation, fast-tracking its regulatory review process.
Meanwhile, private hospitals in Dubai and Singapore are among the first to pilot the system at scale, integrating AI-based diagnostics into routine cancer screening for annual checkups.